Pavilion Publishing and Media Ltd
Blue Sky Offices Shoreham, 25 Cecil Pashley Way, Shoreham-by-Sea, West Sussex, BN43 5FF, UNITED KINGDOM
One of the most significant NHS strikes begins today (13 March), with thousands of junior doctors set to stop all work, including nights, on-call shifts, and non-resident work, for 72 hours.
The strikes come following one of the largest turnouts for a ballot of doctors ever seen. In total, 37,000 out of 47,600 junior doctors voted in the latest ballot, with 98% voting in favour of strike action.
The industrial action is expected to be “hugely disruptive”, with thousands of non-urgent procedures, checks and other appointments cancelled or postponed.
Matthew Taylor, chief executive of the NHS Confederation said the “sheer scale” of the BMA’s ballot outcome, as well as the fact that many health leaders have said that more of their staff have joined unions since the start of this dispute, shows that this is clearly “not a situation that will resolve itself”.
Despite this, the government has been reluctant to engage in any meaningful pay negotiations, with the health secretary, Steve Barclay only offering to discuss pay with the BMA on the evening of Friday 10 March, less than three days before the strikes were due to begin.
Government failed to act quickly enough to stop strike action
His offer also set the precondition that all strikes would be suspended until these discussions took place, something the BMA said would be “completely unacceptable” to its members.
The BMA therefore rejected Mr Barclay’s offer to discuss pay, with Dr Robert Laurenson and Dr Vivek Trivedi, co-chairs of the BMA’s Junior Doctors Committee, describing the offer as a “feeble attempt” to stall the strikes and “kick the can down the road.”
“If you had engaged with us sooner, you would have understood before now that the preconditions you are asking for are the antithesis of our dispute and will not be acceptable to our members,” they said.
Mr Barclay said it was “disappointing” his offer had been rejected, and is now urging unions to come to the negotiating table and “cancel strikes which risk patient safety and impact efforts to tackle the backlog”.
“I want to find a fair settlement which recognises the crucial role of junior doctors and the wider economic pressures facing the UK,” he said.
Why are junior doctors striking?
Unfair pay
The BMA says junior doctors have had their pay cut by roughly a quarter (26%) in real-terms since 2008/09, with newly qualified junior doctors currently earning just £14.09 an hour.
With Pret A Manger bumping up salaries by 19% this year, some baristas will now be able to earn £14.10 an hour. This means you can now “make more money serving coffee than patients”, a BMA advertising campaign states.
This year, junior doctors were offered a 2% increase on their annual wage, but with inflation rising to more than 10%, junior doctor say they are working “more than a month for free”.
The latest NHS staff survey found that only a quarter (26%) of NHS staff were happy with their pay, and 17% of staff were considering leaving the profession for another job.
There is a prevailing narrative that doctors are among the highest earners, but the BMA says it is unfair to compare junior doctors to the whole of the UK, as they spend years in training generating huge student loans and face high exam and professional fees.
Junior doctors have significant work-related expenses
Dr Becky Bates, a foundation year one junior doctor in the East Midlands, explains that postgraduate exams can cost more than £500 a time, and junior doctor also face significant moving expenses as they travel to different cities as part of their training.
Dr Bate says she has racked up more than £100,000 of student loan debt, as well as £15,000 of real debt which she used to cover her fees as a graduate taking on medicine as a second degree. She says she is now relying on her mum to take out credit card debt so that she can keep on top of her expenses.
“As a junior doctor, I can be responsible for more than 400 patients overnight – assessing them, prescribing medication, having difficult conversations with families about end-of-life care, and I can be the first port of call should something go terribly wrong. Yet our skills and responsibilities are being completely devalued.
“My situation is far from unique, and this is why I, and the overwhelmingly majority of my colleagues, have been forced to take to the picket line this week. This is the only option we have left to get the Government to listen to us,” she said.
Working conditions are poor
Junior doctors work long, unsociable hours, including weekends and evenings. Since there are too few doctors in comparison to patients, many work overtime too, and are expected to take on the workload of more than one person, sometimes two.
Junior doctors often put their own health and safety at risk, working in a high stress environment, saving patients’ lives, when they know they could earn more money in an environment where there is less risk and they can work ‘normal hours.
This is on top of substandard working condition, with many unable to get hot food during meal times and some unable to take proper breaks. Furthermore, nearly half of respondents to a BMA survey said there isn’t a mechanism to travel safely to and from work when working out of hours.
The demand on the NHS has increased exponentially since the pandemic, and doctors are also seeing patients with more complex health issues, as well as working with reduced bed capacity and an enormous waiting list.
This can be both physically and mentally exhausting, and in the last 12 months, 78% have felt unwell as the result of work-related stress and 88% said they find their work emotionally exhausting sometimes or always.
Things are getting progressively worse, with more than half (55%) saying their health and wellbeing is worse than a year ago. With working conditions so poor and stress levels so high, the BMA says is this situation is allowed to fester, the implications for patient care will be “far reaching”.
What do the BMA want from the government?
The BMA is seeking restoration of the pay that has been taken away from junior doctors since 2008, which they say stands at 26.1% in real terms.
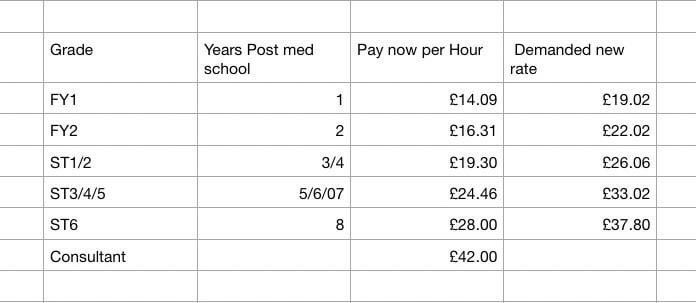
For a junior doctor starting out, this means an increase in their pay from £14.09 per hour to £19.02 per hour, as Figure 1 demonstrates.
Figure 1
This pay increase will cost HM Treasuring £1 billion, just a quarter of what the government spent on unusable PPE during the pandemic, the BMA says.
But Mr Barclay says such a rise is “simply unaffordable”, but says he is determined to find “a fair settlement which recognises the crucial role of junior doctors and the wider economic pressures facing the UK.”
“I’ve been having constructive and meaningful talks with unions representing nurses, ambulance workers and other non-medical staff, which have agreed to pause strike action, and negotiations will continue this week.
“We have been working closely with NHS England on contingency plans to help protect patient safety during strikes, prioritising emergency, urgent and critical care – but there will inevitably be some disruption for patients.”
How will the strikes affect patient care?
Junior doctors account for more than 40% of the medical workforce, and roughly 36,000 junior doctors are expected to strike until Thursday morning.
“Junior doctor” is a broad term that includes doctors that are newly qualified, all the way up to doctors who have 10 years of experience, as Figure 1 demonstrates.
However, one doctor tweeted that with training bottlenecks, this table presents the “best case scenario”, with some spending 10-15 years as a junior doctor, highlighting just how long it takes doctors to work their way up to the top of the profession.
With so many doctors on strike, many of whom are highly experienced, the level of disruption will be significant. Last time junior doctors went on strike, 300,000 outpatient appointments were cancelled.
More than 100,000 appointments have already been cancelled this winter due to the nursing strikes, and while consultants will be brought in to provide some cover, the NHS is warning that thousands more patients will face postponements to their treatment.
The backlog of care already stands at 7.21 million people, with 3 million of these patients waiting for more than 18 weeks, and roughly 379,000 waiting for more than a year. The strikes will only exacerbate these waiting times, which could lead to poorer patient outcomes.
But doctors say they are striking for patients; doctors can only provide good, safe and effective patient care if they are not overstretched and burnt out.
If pay levels remain as they are, more doctors will begin to leave the profession to work abroad or in a different sector entirely, this will put further strain on the NHS, elongating waiting times for care and increasing the risk of mistakes being made.
The Royal College of Emergency Medicine estimates that between 300 and 500 people are dying unnecessarily every week because of the state of emergency departments across the UK. If junior doctors continue to leave the profession in the way they are now, this number will only grow.
As Dr Laurenson and Dr Trivedi highlight, junior doctors are not only striking to restore their pay, but also to restore the workforce and “make the NHS an effective healthcare system again.”


